How might intensity modulated Radiotherapy help you?
Patients who have had a cancer diagnosis may soon find they are discussing a range of treatment options that includes radiotherapy. But while most lay people will have some idea of what radiotherapy is and how it works – usually because they know somebody who has been treated that way – not many will know about the different versions of the treatment.
What the lay person generally knows is that radiotherapy involves using radiation to kill off cancerous cells and tumours, not by zapping them like some laser, but by damaging their DNA so their cells cannot divide and grow.
However, because radiotherapy involves doses of radiation that can also harm DNA in healthy cells and tissues, with a range of side-effects, plus the fact that a more concentrated and accurately directed beam that is better focused on the target area brings better results, specific kinds of radiotherapy treatment can achieve more.
How IMRT Works
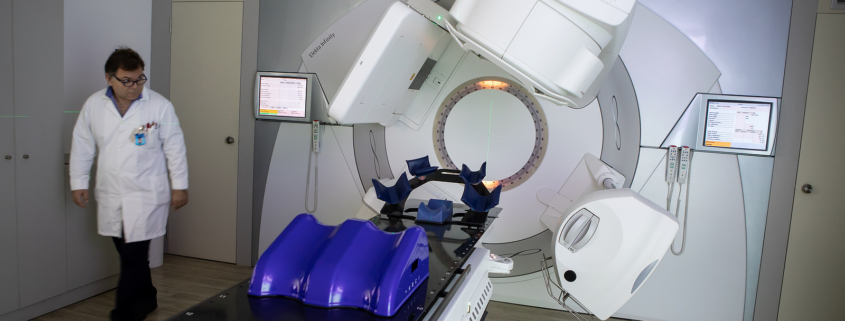
Intensity Modulated Radiotherapy, or IMRT, is a case in point. This is a treatment delivered using linear accelerators controlled by computers, which will deliver a very precise level of radiation to a tumour or even a particular part of the tumour.
The radiation is delivered in small volumes and comes from different angles, highlighting the reality that while scans and images may come out in 2D, tumours exist in 3D and hitting the right spot each time means delivering each dose to the exact spot where it is most needed. Often this is done by using multiple beams simultaneously delivered from different directions.
To ensure this can be done with accuracy, 3D tomography is used in the preparation for the procedure. This will enable the tumour to be mapped out in 3D and the specific areas that need the most intense and precisely calibrated doses of radiation to be identified and their positions pinpointed.
The scanning for this is done by MRI and the calculated dose is worked out by computer, bringing to bear the latest and most advanced complementary technologies to help ensure this form of radiotherapy is delivered in the most adroit and precise manner, something almost unimaginable when radiotherapy was first used in the 1900s.
What IMRT Procedures Involve
All this makes the treatment a lot more complex than other ways of delivering radiotherapy, which necessitates more checks and preparation for treatment, while the treatment itself will last for longer.
However, because there is such a contrast in the dosage received by tumours (where it needs to go) and by surrounding healthy tissue (where you don’t want it to go), it also enables stronger doses of radiation to be deployed in attacking tumours, making it more likely to be highly effective.
What all this means is that some specific forms of cancer are better treated with this kind of radiotherapy, with the patient having to lie still in a particle accelerator while the doses are delivered over a period that may range from 15 minutes to an hour. For those prone to claustrophobia, it can be unpleasant, but life-saving.
New Research Breakthrough For IMRT
The benefits of IMRT may be about to grow as new research has shown how it can be used to achieve a ‘gold standard’ of treatment for those suffering cancers of the head or neck and help avoid dysphagia, a condition where a person has difficulty swallowing.
A trial at the Royal Marsden Hospital in London, co-ordinated by the Cancer Research Trust, set out to compare the side effects of dysphagia-optimised intensity modulated radiotherapy (DO-IMRT) with standard forms of IMRT.
A key side-effect issue that can occur in this case is that the delivery of radiation to the muscles involved in swallowing can cause dysphagia. Some patients may need to have a permanent feeding tube inserted.
The study compared how often newly-diagnosed throat cancer patients treated with each form of IMRT suffered dysphagia. The result, published in the Lancet, was that of the 112 patients, half of whom received DO-IMRT and the others standard IMRT, there was a clear difference in the ability to swallow.
Among the DO-IMRT group, 62 per cent were able to eat at least some food that needed chewing and 85 per cent felt comfortable eating in public. In the other group, the respective figures were 45 per cent and 75 per cent. All this happened while there was no significant difference in the three-year survival rate between the two groups.
This discovery means that, in future, IMRT for patients of neck and head cancers can be delivered in an even more precise manner, in order to further limit its side effects without having any negative impact on patient outcomes.