How Radiotherapy Aids in Improving Cancer Survival Rates
When private radiotherapy was first used to treat cancer patients in the early 20th century, it was as a means of palliative care to ease the suffering of the dying. While it is still often used this way today, for most of the past century, it has also had a role in extending life and, in some cases, defeating cancer altogether.
Outcomes for patients will depend on a range of factors, from the type of cancer to age and, most importantly, how early the cancer is diagnosed. Nonetheless, two factors have become increasingly prevalent in recent years. One is that there are more diagnoses, while the other is an increase in successful treatments.
Cancer Rates Up – But So Is Survival
The latest UK data has highlighted this. Cancer Research UK’s Cancer in the UK report, published this month, revealed that over the past 50 years, the proportion of people in Britain being diagnosed with cancer has risen by 47 per cent. However, the mortality rate has fallen by 22 per cent over the same period.
Most notably, the proportion of people who get cancer but survive at least another ten years is now one in two, compared with one in four in the early 1970s.
The diagnostic element is an important factor, as better and earlier detection is important in tackling cancer, in particular by treating it before metastasis takes place – the point at which cancer cells break away from the area initially affected and migrate to other parts of the body.
At the same time, there are other reasons for an increase in diagnoses, not least an ageing population.
The Global Picture
The UK situation is anything but unique. Survival rates are improving around the world thanks to improved diagnostics, but also more advanced treatments. Indeed, data published by the World Population Review has shown that some countries are outperforming Britain, and indeed other Western countries, in many areas.
For example, the highest five-year survival rates for stomach cancer are to be found in South Korea, followed by Japan and Jordan. Europe is also outperformed by Japan, the US and others in lung cancer survival. However, in breast cancer, the survival rate in most European countries is over 80 per cent. Prostate cancer survival rates are higher still.
Across the globe, these figures will be much more favourable than they were not just half a century ago, but more recently. Moreover, while ageing populations and advances in diagnostics make higher case rates likely in the coming years, survival rates can be expected to continue to improve as new and better treatments emerge.
The Role Radiotherapy Plays In Better Outcomes
The improvements in treatment have certainly not all come from radiotherapy, with other kinds of therapy and new drugs emerging with great regularity. Nonetheless, the advancement in the use of radiotherapy has made a huge difference.
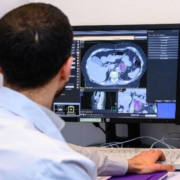
This has included the use of more focused stereotactic radiosurgery that can target precise areas such as tumours without harming sensitive surrounding tissue (a particular priority in brain cancer cases), plus the advancement in scanning techniques to enable better targeting and monitoring of the delivery of radiation.
Further benefits can arise when the calibration of doses is aided by technological advances and research indicating how high (or low) a dosage may be beneficial in various circumstances, through a better understanding of the balance between the benefits of treating the cancer and any associated side-effects of treatment.
Austrian Research Offers Lung Cancer Breakthrough
Among the very latest developments has been research showing that high-dose radiation therapy can improve prospects for lung cancer patients without increasing the risk to the patient. This was the conclusion of a study run by Karl Landsteiner University of Health Sciences, in the Austrian city of Krems, the journal Cure Today reports.
Pulmonologist Dr Felix Schragel explained that the postulated risk was that higher doses of radiation might lead to more pneumonitis cases, which manifests in the form of dangerous lung inflammation. However, the study showed that patients given higher doses actually had lower rates of pneumonitis.
Furthermore, the data indicated a higher survival rate for lung cancer patients given the higher dose, with a 93 per cent one-year survival rate for those who had the higher dose, which remained steady after four years.
This research could help improve outcomes for patients with lung cancer when undergoing radiotherapy treatment. In the same way, patients with brain, prostate, breast, neck and other cancers may similarly benefit from other recent – and future – advancements in treatment.
Radiotherapy is not new, but the understanding of how best to deploy it and the technology to deliver it in the right amounts and precise locations are continuing to advance. In using the latest technology and insights, we aim to get the best possible outcome for every patient.
Learn more about our advanced radiotherapy treatments for different cancers on the Amethyst Group website.