What Is Brachytherapy And When Is It Used To Treat Cancer?
Treating cancer using radiation therapy is about using precisely managed and targeted radioactivity to destroy malignant tissue whilst sparing healthy tissue surrounding it.
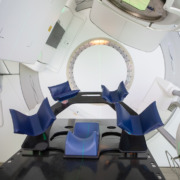
In some cases, this is undertaken using an external radiotherapy beam, such as with the Gamma Knife method. However, there are other cases where the most precise way to deliver doses of radiation is from within using brachytherapy.
Also known as internal radiation, brachytherapy is often used to provide high-dose radiotherapy safely and in a short space of time, but exactly when and where it is most appropriate to use it will often depend on the needs of an individual person and their particular diagnosis.
What Is Brachytherapy?
Brachytherapy uses a source of radiation placed close to the cancer or to where a cancerous tumour has been removed following surgery.
The name brachytherapy comes from the Greek word ‘brachys’, which means ‘short-distance’, and unlike external beam radiotherapy, which often has to pass through several layers of tissue and body matter before reaching a tumour, brachytherapy is placed close to or directly onto the cancer itself.
There are multiple forms of brachytherapy, but they are typically categorised as either high dose rate (HDR) or low dose rate (LDR) which are either temporarily applied or implanted in the body respectively.
HDR brachytherapy usually involves the use of an applicator tube or needle inserted into the body before a radioactive material travels towards it and remains there for as little as five minutes before returning to the source.
By contrast, LDR involves the implantation of radioactive seeds, discs or other tiny pieces of material typically smaller than a grain of rice. This is typically applied using wires or needles and can be either temporary or permanent depending on the type of treatment.
When Was Brachytherapy First Used?
Brachytherapy is the first practical form of radiotherapy, as whilst experimental treatments using X-rays were tried mere months after Wilhelm Roentgen’s discovery, the use of radioactive materials was suggested in 1901 by Pierre Curie.
The use of radioactive seeds, initially made from radium sulphate, was pioneered in the early 1900s thanks to the work of William Duane, and a very similar system of application is still used to this day.
Before the development of external-beam radiation, CT and MRI scans which allow modern forms of external radiotherapy to be accurate and safe, brachytherapy was the standard treatment path for several forms of cancer.
Whilst its uses are more specific today, it still has some advantages that make it a viable option for oncologists in certain cases.
What Are The Advantages Of Brachytherapy?
There are several advantages to using brachytherapy, both in HDR and LDR forms, as they can provide higher doses of radiation with a greater degree of flexibility or adaptation compared to some types of external beam radiotherapy treatment.
Brachytherapy is inherently localised; the radiation source is placed directly on the cancer or as close as possible, which means that healthy tissue is less exposed to radiation, reducing potential damage and recovery times.
This localisation can also reduce treatment times significantly; whilst some radiotherapy treatments can take several hours, brachytherapy can take as little as five minutes and typically takes no more than 20, which allows for multiple treatments per day or for a course to be completed more quickly.
As well as this, in cases where the tumour shifts position in the body, something that can be common with cancers that affect the digestive, urinary and reproductive systems, the radioactive implants will move with the cancer and stay in the same position.
Both of these elements reduce the ability of cancer cells to recover and multiply between treatment sessions, and this can sometimes mean that a treatment that would ordinarily require a patient to spend time in a hospital can be completed in an outpatient setting.
When Is It Used To Treat Cancer?
It is typically used to treat cancers within body cavities or close to the skin, with the most common treatments focusing on cancers of the cervix, prostate, skin and breast. The easier it is to access a tumour, the greater the chance that brachytherapy can be used.
Generally, it is used to treat early-stage cancer before it has a chance to spread or metastasise, as it is a well-known, advanced, safe and often painless procedure, or it can sometimes be used following other more intensive cancer treatments to destroy any lingering cancer cells.
Permanent low-dose seed implantation is a standard treatment for localised prostate cancer, as it is less invasive than other treatments and a person can return to normal in just a few days.