Biomarkers May Reveal Radiotherapy Effect On Rectal Cancer
Rectal cancer is more than just a literal pain in the rear end; it is a potentially deadly condition that can prove very unpleasant to treat, not least because until now there have been no available biomarkers to indicate how effective radiotherapy is in tackling it.
As Medical Express reports, however, that may be about to change thanks to new research involving several universities across the UK and Europe, which could mean that before too much longer, some patients will not need to undergo surgery after getting treatment at a radiotherapy centre.
Although it is standard practice for patients with advanced colorectal cancer to receive radiotherapy and then undergo surgery, in 15 per cent of cases the radiotherapy leads to the cancer disappearing completely before they go under the knife.
However, these patients have not been spared surgery due to the lack of reliable biomarkers from their tissues, blood, or any other body fluid to show that the cancer has gone and surgery is not required. This means some patients will end up having operations when it is not actually necessary for them to be cancer-free.
The Search For Biomarkers
This issue is something the S:CORT consortium, led by Oxford University Professor Tim Maughan, set out to tackle in 2015, aiming to find one or more reliable biomarkers that could enable some patients to complete their treatment using radiotherapy alone without having to undergo surgery and subsequent recovery.
The S:CORT consortium included researchers from Oxford alongside colleagues at University College London and the universities of Leeds, Aberdeen, Birmingham, Belfast and Berne. The work has unveiled some promising findings, with several potential indicators now emerging.
A trio of studies involving 826 patients and leveraging the power of machine learning has established three possible biomarkers, with results being published in the journals eBiomedicine and Cancer Research Communications.
Three Biomarker Possibilities
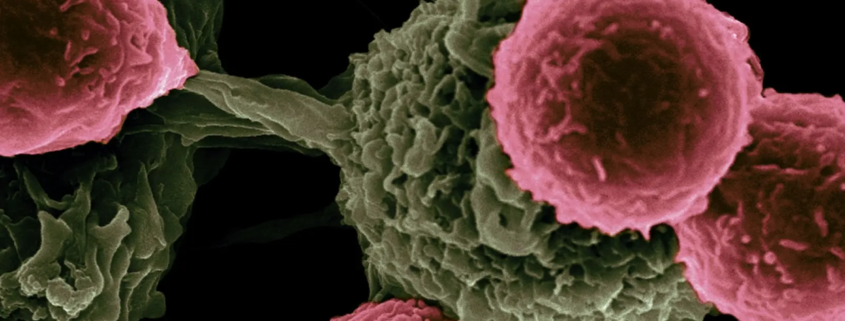
Firstly, the research found that tumours themselves offered a clue, as it was only in tumours that included particular kinds of supportive tissues and immune cells that a complete response to radiotherapy (that is, the elimination of the tumour) can occur.
Secondly, machine learning found that a predictive model with an accuracy level of 80 per cent could be established, based on the expression of 33 genes that can predict treatment outcomes.
A third discovery emerged from the image analysis of biopsies, which also used artificial intelligence.
This assigned particular molecular subtypes to tumours. One of these subtypes, called imCMS1, was linked to a higher probability of cancer being eliminated by radiotherapy, whereas another subtype, imCMS4, was connected with the opposite outcome.
The Next Steps
Needless to say, much more research will be needed before any of these can be confirmed as reliable biomarkers that can obviate the requirement for surgery in some colorectal cancer patients, but the day when that is the case has certainly come a lot nearer. New trials will now be carried out involving patients undergoing radiotherapy.
Professor Maughan said: “These studies provide a deeper understanding of the biological factors that influence radiotherapy response in rectal cancer,” adding that they hint at new immunotherapeutic treatments as well as improved treatment outcome prediction models.
Honorary Clinical Chair in Oncology and Consultant Oncologist at NHS Grampian, Professor Leslie Samuel, commented that the research results are “good news for patients who wish to avoid surgery, as they offer a good opportunity to identify these patients most likely to be able to avoid radical surgery”.
Implications For Patients
While the research clearly has some way to go, it may even benefit some people who are current patients. This is because rectal cancer is one of the slower conditions to develop, taking around 10-15 years for the first signs – a clump of cells known as adenomas – to develop into full tumours.
This sometimes means, of course, that the condition is detected early and the polyps removed, which prevents them from progressing to full rectal cancer and means no radiotherapy is needed. If you are a patient needing radiotherapy, it will be because it has progressed well beyond that point.
Symptoms like bleeding, constipation, abdominal pain and weight loss are among the symptoms that can point to the possibility of colorectal symptoms, which does enable many patients to have the condition diagnosed and treated early.
However, given where it is in the anatomy it may be one of those conditions nobody wants to discuss with their doctor, leading to a reluctance to seek a diagnosis. Nonetheless, research has shown cases have been rising among younger people, making diagnosis more important than ever.
Whatever the circumstances, if you are a patient with this condition, you may be among those to benefit in the future from the use of biomarkers after radiotherapy that can show you won’t need the additional pain and inconvenience of surgery.